Blood Pressure - Why Should You Care
We have all heard the term and probably know that it’s one number over another number and it must be a marker of health that’s important because your doctor checks it every time you are at the office. And if you’re like millions of Americans, you’ve been monitoring it at home and might be taking medicine for it.
But do you know what it really is measuring and do you know why you should care that it is high? In this blog post I dive into:
what is the pressure we are measuring and talking about
why is it bad when that pressure is high
the consequential effects of chronic high blood pressure throughout the body
what can you do besides taking medication to help lower it (lifestyle modifications)
what type, amount, and intensity of exercise can reduce blood pressure
how can I as a physical therapist with a degree in nutrition science help you build habits to prevent high blood pressure before it starts
how can I help you exercise without pain and keep you accountable to healthy eating, sleep, and stress reduction as part of a healthier you (while reducing your blood pressure!)
Blood Pressure - What is it?
Medical definition: a measure of arterial pressure in mmHg.
Meaningful definition: the force of blood pushing against the walls of your arteries.
Blood pressure measures the amount of pressure in your arteries during heart muscle contraction (systolic) AND the amount of pressure in your arteries during heart muscle relaxation (diastolic). It is a very common key measure of function and health in your cardiovascular system.
Let’s back up a minute - and review the cardiovascular system, aka the circulatory system. They both refer to the same system of organs that transports blood throughout our entire body, to all of the other organs who require blood in order to function. Our heart pumps blood into the arteries to be delivered to other organs. Our veins return blood from our organs to the heart, to be re-oxygenated by the lungs before being pumped out again to our body. Blood is the fluid of life, transporting nutrients and necessary enzymes, hormones, and molecules to places of need and removing waste once the organs have used what they want. Blood flows in the infrastructure vessels of arteries and veins as a result of gravity, pressure, and heart muscle contractions. (Thank goodness we don’t have to manage all of this work consciously!)
The heart is a muscle made up of 4 chambers and valves, that coordinate to receive and eject blood. Blood from our veins enters the heart in the right atrium and gets pushed out to the lungs to get oxygen by the right ventricle. Blood is always received by an atrium, the entering hall if you will, then moves to the ventricle where it waits for a contraction to be pushed out of the heart. The lungs return the now oxygenated blood to the left atrium, then it flows into the left ventricle where it gets pushed out by the strongest heart chamber contraction into an artery to travel to the rest of the body. To be fair, the atrium contracts to push the blood into the ventricle, it doesn’t just flow without effort through open valves, but its not needed to be as strong as the ventricle.
To review:
Systolic Blood Pressure: the force of the blood against artery walls when your heart beats (top number)
Diastolic Blood Pressure: the force of the blood against artery walls when your heart is at rest between beats (bottom number)
[The difference between these two numbers is called your pulse pressure, which helps indicate various heart conditions, in addition to blood pressure. ]
Why is blood pressure important?
Adequate blood pressure is necessary to pump blood throughout your body effectively and to attenuate quickly with positional changes. For example, have you ever "stood up too fast" and felt dizzy or lightheaded for a few seconds? You experienced a small momentary drop in blood pressure as your body tries to quickly adapt to a change in gravitational forces. Chronic low or high blood pressure is problematic for your entire circulatory system. So check your blood pressure often to make sure it is normal: <120/<80.
What do the numbers mean?
As the force increases, or as the number gets higher, that means there is more pressure in the arteries from the blood pushing against the walls, either at rest (diastolic) or during heart muscle contraction (systolic).
The ACC (American College of Cardiology) and the AHA (American Heart Association) have created staged hypertension categories based on research looking at risk for & prevalence of various diseases as well as mortality from heart related causes. (see chart in photo below)
SBP = systolic blood pressure. DBP = diastolic blood pressure
Hypertension is the same as saying high blood pressure. Hypertension is often shortened to HTN. Unless you’ve been “living under a rock”, you’ve probably heard from somewhere that hypertension is bad. But why?
Why is High Blood Pressure a Problem?
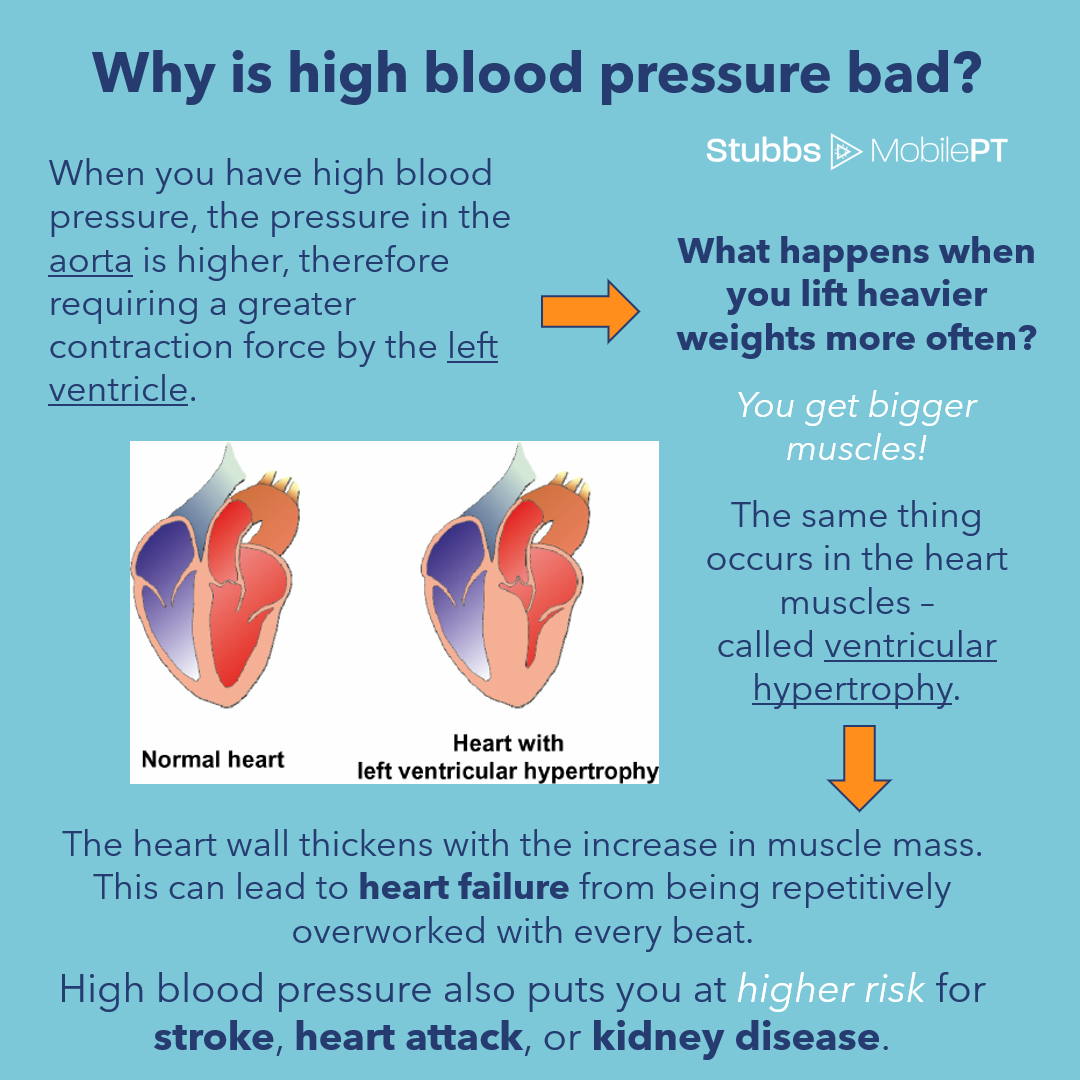
The left ventricle chamber of the heart must contract hard enough to open the valve to eject the blood out of your heart to circulate in your body. What determines how hard it contracts? The amount of pressure in the walls of the aorta, which is just on the other side of the valve and is the largest artery in our body. The heart (left ventricle) must contract at a force creating a pressure greater than the pressure in the walls of the aorta in order for the valve to open. So when your blood pressure is higher, the left ventricle (heart) must contract even stronger.
When we contract repetitively at a high force, we build muscle. Right? That's why we work out.
The same muscle building occurs in the heart muscle, but excessive mass of muscle in the heart is problematic, termed ventricular hypertrophy. The muscle mass can start to encroach on the open space in the chamber, meaning less space for blood. That means with less volume of blood per contraction, in order to push out the same volume of blood around your body, the heart has to beat MORE times, at a STRONGER force.
The artery walls also experience a higher than normal pressure during hypertension. When pressure is higher against the artery walls, they change in cell structure and become more likely to bind plaque deposits. Plaque deposits can cause physical obstruction to the flow of blood, narrowing the vessel diameter. They can also lead to hardening of the arteries, making them less flexible & resilient, called atherosclerosis.
Are those changes really that bad?
In combination, both of these changes can lead to even greater increases in blood pressure against the artery walls, therefore requiring the heart muscle to work harder with every beat. Traveling clots in the blood can get caught by the narrowed and less flexible artery vessels. Plaque deposits can sometimes break off in a small piece which results in clot forming along the wall of the artery where it once was. Clots that block the entire width of the vessel impede blood flow to your organs. The heart is a muscle that also must be fed by arteries bringing blood, and if you experience a clot in one of these arteries blocking blood flow to your heart muscle, you experience a heart attack. Clots & arterial plaque deposits can also cause ischemic events (due to lack of blood flow) in the brain which are called a stroke. Anytime there is a prolonged absence of blood flow to any tissue or organ, ischemia occurs leading to cellular & tissue death and loss of function.
So its not just my heart?
High blood pressure not only affects your heart, but stimulates negative changes to the other organs it is sending blood to, like your eyes, kidneys, and skin. This is why it is important to monitor BP consistently to observe any consistent increases so that you can take quick action to make lifestyle modifications, or start taking an anti-hypertensive medication. The longer you can maintain normal pressures in your arteries, the healthier and longer-lasting the rest of your organs will be.
And what about low blood pressure?
Chronic abnormally low blood pressure (hypotension) commonly defined as 90/60 or lower also leads to problems. It can result in inadequate blood flow to organs resulting in dizziness, lightheadedness, fainting, blurred vision, nausea, fatigue, and lack of concentration. All of these symptoms greatly increase your risk for falls, which can result in musculoskeletal injuries. Mild dehydration can even lead to mild symptoms of low blood pressure. Low blood pressure without symptoms is not generally considered a problem, but your doctor may want you to monitor it consistently. Hypotension can also emergently occur from shock, common after trauma or loss of blood, and is an emergent condition, immediate treatment is needed.
So what can you do to prevent high blood pressure?
What lifestyle modifications can you make?
Exercise is a big one, with demonstrable effects at reducing blood pressure, but there are others too.
Lifestyle modifications include consistent exercise, avoiding sedentary habits, being more physically active, reducing sodium intake, eating whole foods, following a DASH or heart healthy diet (like the Mediterranean Diet), limiting saturated fat intake, lowering cholesterol, and reducing stress.
You can also choose to make these lifestyle choices when you are younger as a preventative measure; start saving yourself for retirement now. Avoid or delay the onset of hypertension that requires pharmaceutical management; medications have so many potential negative side effects. You also want to limit your reliance on medications, because after 5 (meaning 5 daily or regular prescriptions), your fall risk increases!
How does Exercise Help?
Exercise can help reduce your blood pressure. During exercise there is a normal gradual increase in systolic blood pressure and a slight gradual decrease or no change in diastolic blood pressure. Immediately after exercise up to 24 hours post-exercise, a reduction in blood pressure by an average of 5-7 mmHG occurs. That means you saved your heart from having to work as hard each beat for up to one day after you exercise!
What kind of exercise is best?
Your favorite kind of exercise is best. Because you will be the most likely to do it. :)
Research comparing aerobic exercise, resistance exercise, or combination exercise plans saw similar positive results with decreasing blood pressure. On average, therefore, one isn’t better than the other at reducing blood pressure. They do have other benefits and should align with your fitness or functional goals.
What is important with the exercise you choose is to do it 20-30 minutes per day with a minimum of 90 total minutes per week at a moderate - high intensity. High intensity exercise is not required, as exercising at 55% of your heart rate max provides the beneficial effects on blood pressure and cardio protection. A good way to ensure moderate intensity exercise, is that it should be mildly difficult to continue to carry a conversation. You can also calculate your heart rate max by subtracting your age from 220 and then multiplying that value by .55 to determine a target heart rate for moderate intensity.
One research study investigating the effects of consistent aerobic exercise on stage 2 hypertension found that blood pressure values could be reduced to stage 1 levels in 12 weeks. The participants performed moderate intensity aerobic exercise for 30-45 minutes on 3 or more days per week and average blood pressure changed from 145/85 to 137/80 in 3 months.
Be thankful for your cardiovascular system and all the great things it does behind the scenes to sustain your life!
So Why is a Physical Therapist Writing About Blood Pressure?
Because I believe the more you know, and the earlier in life you know it, the sooner and easier it will be to make changes that affect your health in life.
As a physical therapist in typical clinic settings, we see people struggling with the effects of multiple chronic diseases and the added challenges they have in recovering from aches, pains, injuries, surgeries, and hospitalizations. With multiple chronic diseases, especially anything related to the heart, prognosis is more guarded and protracted. Make it easier on yourself to recover from bodily pain or injury, by living a heart healthy lifestyle to maintain normal blood pressure.
We (PTs) are uniquely trained in all of the following:
blood pressure measurements,
assessing blood pressure response to exercise for cardiovascular safety,
creating & monitoring exercise plans to improve cardiovascular fitness,
understanding & treating orthopedic musculoskeletal conditions affecting exercise tolerance
adapting specific exercise around pain & functional limitations,
instructing exercises to improve pain & function while maintaining cardiovascular and balance safety, and
dosing exercise & progressions to ensure desired bone, muscle, tendon, ligament changes while avoiding training error.
If you could benefit from this combination of knowledge and services, then a physical therapist is who you need to see!
I, Lauren Stubbs, PT am uniquely trained in:
nutrition science
educating general nutrition needs and concepts
reviewing current food intake habits
assessing food intake against nutrition standards and your goals
recommending food swaps, recipes, recipe modifications
guiding, motivating, celebrating, and holding you accountable to small weekly habit changes
incorporating sleep, stress management, hydration, pain relief, movement, exercise, and healthy eating improvements into your individualized plan and coaching sessions.
You can get any or all of the above services during physical therapy, fitness & wellness, or annual wellness visits at Stubbs Mobile Physical Therapy. We serve busy active professionals, parents & retirees helping them eliminate acute and chronic pains while taking the hassle out of appointments. No scheduling time out of work to drive to the appointment, dealing with traffic and directions, finding parking, filling out paperwork, nor sitting in a waiting room. My personalized service saves you time in 2 ways and improves outcomes making recovery more efficient and injury prevention more likely. By coming to your home or office we eliminate the time & hassle of traveling and our clients experience sustained pain relief with an average of 4-6 visits vs a traditional average of 8-12.
Are videos more your learning style?
Check out this simple but engaging animated youtube video from TED Ed on blood pressure.
Additional Resources
The New (2017) Hypertension Stage Guidelines https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
Lifestyle Modifications Details https://journals.lww.com/acsm-healthfitness/fulltext/2018/09000/lifestyle_modifications_to_promote_healthy_blood.4.aspx
Health Issues and Diseases linked to Hypertension https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20045868